GI-MAP’s qPCR Technology Identifies C. difficile in a Long-Suffering Patient

Elderly Patient with Chronic, Unresolved GI Complaints Turns to Functional Medicine
Diane is an 83-year-old female who was referred to our clinic for a consult by her gastroenterologist. Diane presented to the office complaining of chronic diarrhea, severe abdominal pain, daily belching, malodorous gas, and bloating. Diane's chronic intestinal pain was so disruptive that she avoided eating. As a result, she had lost thirty pounds, unintentionally, over the course of two years.
When I first saw Diane, she was experiencing urgent, watery diarrhea three to five times per day, accompanied by a significant amount of gas. She did not report any blood or mucus in her stool. After talking with her, I discovered that many of Diane's gastrointestinal (GI) complaints began over two years earlier after being treated with multiple rounds of antibiotics for suspected urinary tract infections. I immediately ordered a GI-MAP™ stool test for further analysis.
GI-MAP is a Non-Invasive Stool Test That Can Identify Low-Level Pathogens Other Tests and Invasive Procedures May Miss
Before visiting my office, Diane had seen a gastroenterologist who performed a colonoscopy, an endoscopy, and a SIBO (small intestinal bacterial overgrowth) breath test. The colonoscopy and endoscopy results were normal, and the SIBO breath test was negative, but Diane's chronic gastrointestinal symptoms persisted.
Just prior to her first visit with me, Diane went to the emergency department because her acute abdominal pain had worsened. The hospital performed GI pathogen testing as well as a CT scan, and all findings were negative.
Within two weeks, we received the GI-MAP results, and the root cause of her discomfort became obvious. She had Clostridiodes difficile (formerly known as Clostridium difficile). Diane's GI-MAP results showed an elevation of both C. difficile Toxin A and Toxin B.

In this case, the GI-MAP identified the root cause of Diane's symptoms that were missed by more expensive and invasive conventional procedures. The GI-MAP uses quantitative PCR (qPCR) technology which is more sensitive than the standard PCR run in the hospital, which explains why it was missed in the ER.
Understanding C. difficile
Clostridiodes difficile (C. diff.) is a gram-positive anaerobic bacterium that causes antibiotic-associated colitis. It can colonize the intestine following a disruption of normal gut flora.1 C. difficile can present anywhere from asymptomatic carrier state to significant disease with megacolon.2 To properly diagnose an active infection of C. difficile, a positive C. difficile Toxin B is key. While Toxin A can cause issues, Toxin B always causes issues and is significantly more virulent.3 Once a symptomatic patient is identified through the GI-MAP's quantitative PCR technology, then verification of direct testing for C. difficile toxins is helpful to understand how to move forward with treatment.4 If diarrhea, positive PCR, and positive Toxin A or B are all present, more aggressive antibiotic treatment is warranted. Since the PCR test for the toxins does not differentiate between the carrier state and an active infection, to move forward with treatment, both a PCR and toxin panel are necessary.
Treatment and Symptom Resolution of C. difficile Using GI-MAP
Once we found the positive Toxin B in addition to the GI-MAP results, I began standard treatment with Vancomycin as well as probiotic support utilizing both Saccharomyces boulardii and a Lactobacillus-based probiotic.5
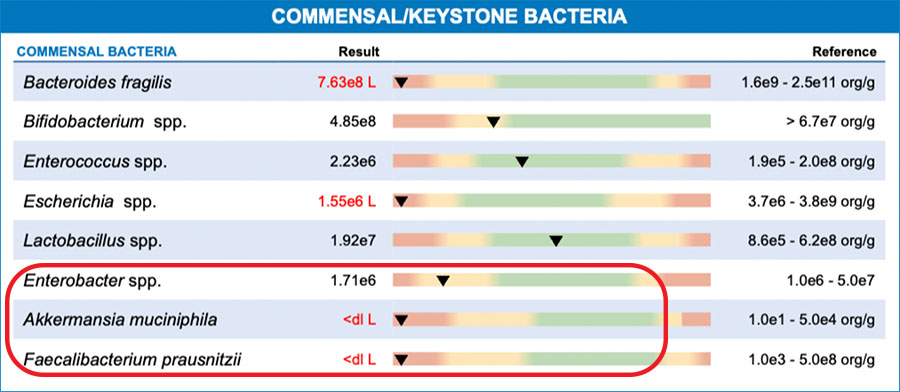
Almost always, when we identify C. difficile infection on the GI-MAP, we also see very low commensal flora and keystone species. This was also the case with Diane's results—particularly low levels of butyrate-producing species. It is important to support these commensals while addressing the infection.
Following her treatment protocol, many of her symptoms resolved. Diane no longer complained about belching, passing malodorous gas, or abdominal pain. Thanks to GI-MAP screening, we found positive findings that did not show up through less sensitive testing. Diane does, however, remain at risk for re-infection with C. diff. We discussed at length that she is now a carrier. Avoiding unnecessary antibiotics as well as practicing good hygiene are her best tools to prevent re-infection, which occurs in one out of every six people who have a C. diff infection. Because she was symptom free, I did not repeat the GI-MAP. However, if she begins to experience any discomfort with digestion, then a retest would be warranted to see how much her microbiome had shifted post infection.
The GI-MAP allowed us to properly diagnose and treat Diane. This fundamentally improved her quality of life, and she is exceptionally grateful.

Ilana Gurevich, ND, NSOM, FABNG
Dr. Gurevich is a naturopathic medical physician and an acupuncturist who uses individualized natural therapies to address the underlying cause of disease. She encourages her patients to take an active role in their own health care. Dr. Gurevich relies on a variety of natural modalities including Chinese and Western herbal medicine, acupuncture, nutritional supplements, homeopathy, hydrotherapy, and dietary education.
The opinions expressed in this presentation are the author's own. Information is provided for informational purposes only and is not meant to be a substitute for personal advice provided by a doctor or other qualified health care professional. Patients should not use the information contained herein for diagnosing a health or fitness problem or disease. Patients should always consult with a doctor or other health care professional for medical advice or information about diagnosis and treatment.
REFERENCES
- Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015 Jan 27;313(4):398-408. doi: 10.1001/jama.2014.17103. PMID: 25626036; PMCID: PMC6561347.
- Kelly CR, Fischer M, Allegretti JR, LaPlante K, Stewart DB, Limketkai BN, Stollman NH. ACG Clinical Guidelines: Prevention, Diagnosis, and Treatment of Clostridioides difficile Infections. Am J Gastroenterol. 2021 Jun 1;116(6):1124-1147. doi: 10.14309/ajg.0000000000001278. Erratum in: Am J Gastroenterol. 2022 Feb 1;117(2):358. PMID: 34003176.
- Riegler M, Sedivy R, Pothoulakis C, Hamilton G, Zacherl J, Bischof G, Cosentini E, Feil W, Schiessel R, LaMont JT, et al. Clostridium difficile toxin B is more potent than toxin A in damaging human colonic epithelium in vitro. J Clin Invest. 1995 May;95(5):2004-11.
- Gerding DN, Johnson S, Peterson LR, Mulligan ME, Silva J Jr. Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995 Aug;16(8):459-77. doi: 10.1086/648363. PMID: 7594392.
- Goldenberg JZ, Ma SS, Saxton JD, Martzen MR, Vandvik PO, Thorlund K, Guyatt GH, Johnston BC. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2013 May 31;(5):CD006095. doi: 10.1002/14651858.CD006095.pub3. Update in: Cochrane Database Syst Rev. 2017 Dec 19;12 :CD006095. PMID: 23728658.
- https://www.cdc.gov/cdiff/after.html