Insufficiency Dysbiosis: A Case Study

Joseph, a 60-year-old man, presented to the clinic with a persistent history of gas and bloating. These symptoms began long before he immigrated to the United States 15 years ago. Growing up traveling extensively, Joseph experienced frequent foodborne illnesses and a significant history of antibiotic use during childhood and early adulthood. To this day, he uses antibiotics one to two times annually due to infections contracted during his frequent travels.
Joseph’s primary complaint was excessive nighttime belching, which disrupted his sleep and often necessitated a bowel movement to alleviate the symptoms. His gas production had increased and taken on a sulfurous odor, with belching frequently bringing up the taste of recent meals. He also reported daily bloating, sometimes starting as early as waking. Despite previous treatments for small intestinal bacterial overgrowth (SIBO) and intestinal candidiasis, his symptoms remained unchanged, and his latest SIBO test, conducted two months prior, was normal.
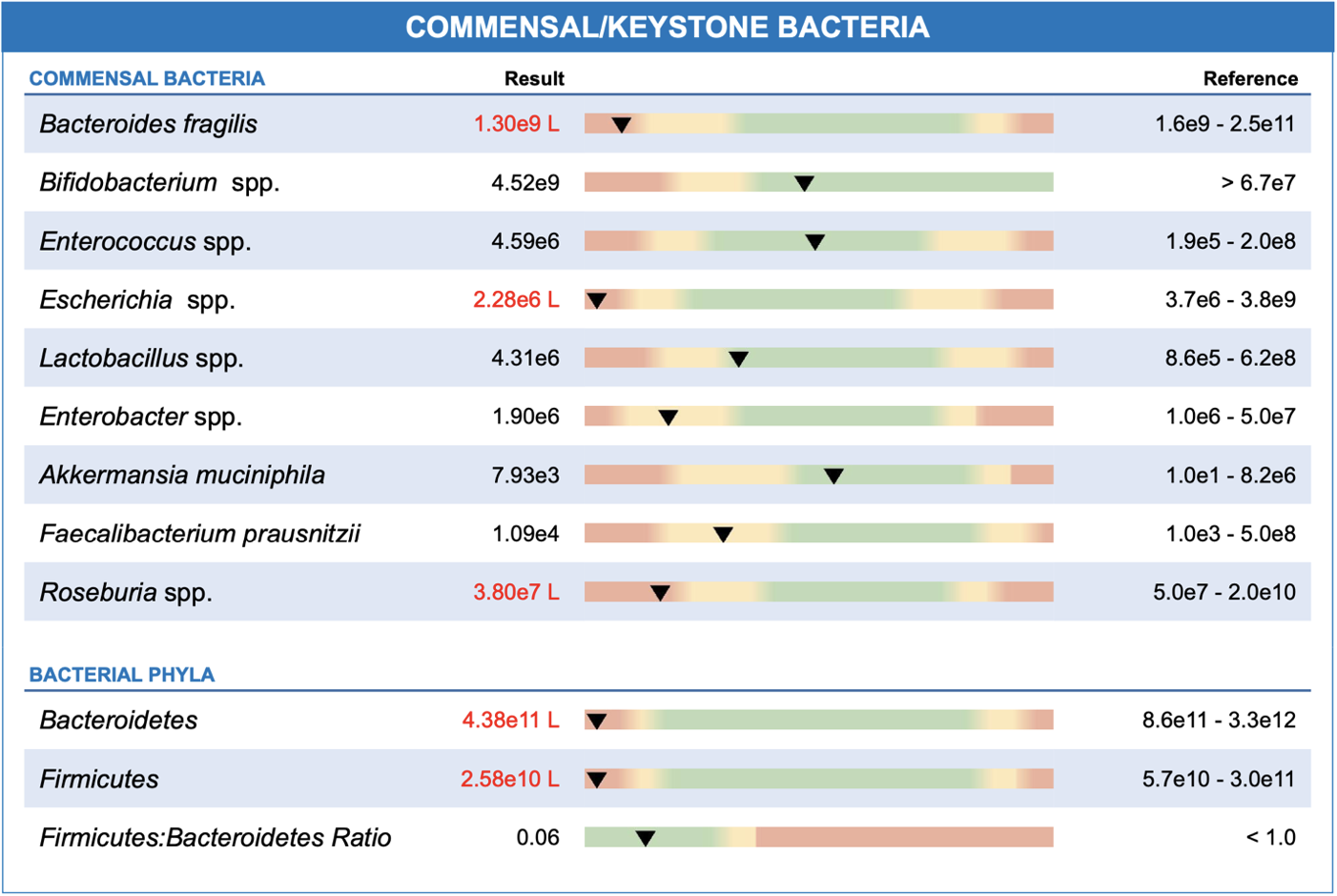
To investigate further, we ran a GI-MAP® stool test, which revealed Joseph was suffering from insufficiency dysbiosis — a condition characterized by low abundance of commensal and keystone species of microorganisms in the gut.
Understanding the Gut Microbiome: Key Insights Into Digestive Health and Well-Being
As Hippocrates wisely said, “All disease begins in the gut.” Modern research continues to link gut health to a wide range of symptoms and conditions. The gut microbiome is an ecosystem of microorganisms essential for digestion, nutrient absorption, and immune function. A diverse microbiome fosters resilience against disease, while a low-diversity microbiome — such as seen in insufficiency dysbiosis — leaves the gut vulnerable to environmental stressors, pathogenic colonization, and opportunistic overgrowth, and reduced recovery after disturbances like antibiotic use.1
Joseph’s GI-MAP test highlighted:
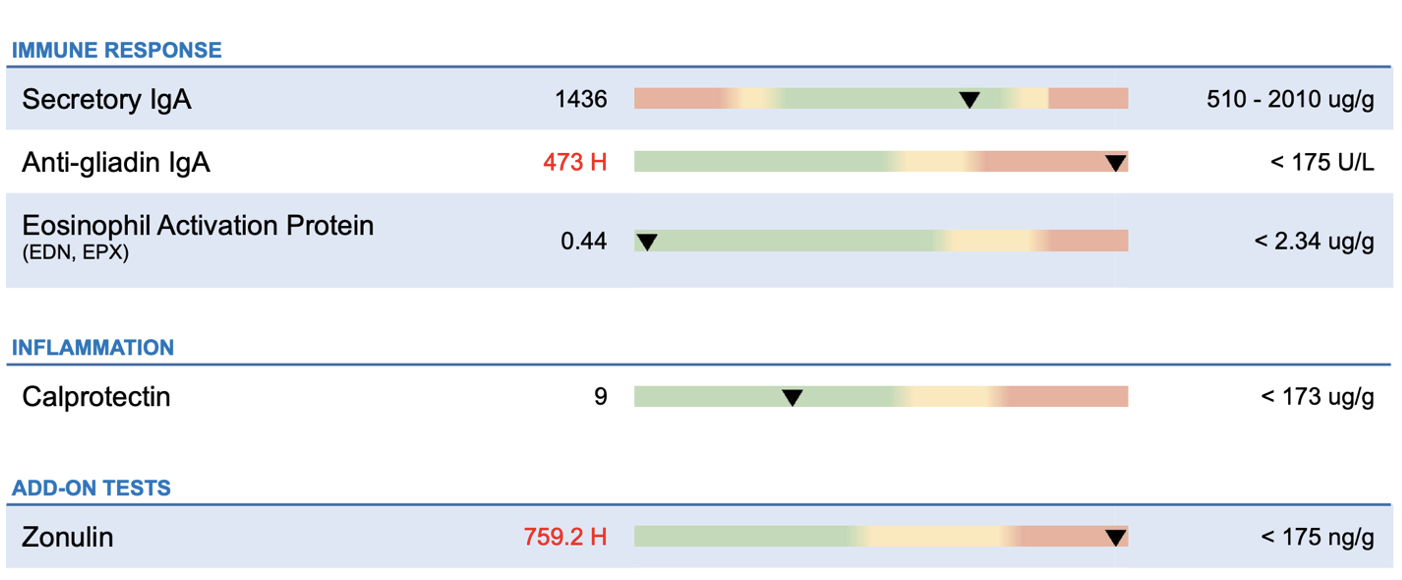
- Elevated zonulin, indicating increased intestinal permeability (commonly known as "leaky gut").
- High anti-gliadin IgA, suggesting a significant sensitivity to gluten.
- Low quantification of key commensal bacteria.
With insufficiency dysbiosis, we often see altered intestinal permeability, potentially leading to "leaky gut" and a reduced capacity for digesting complex carbohydrates and producing essential nutrients.2 Due to this, we see an increased amount of fermentation in the GI which leads patients, like Joseph, to experience more bloating and belching as well as discomfort during the day.
A Targeted Treatment Plan
To address these findings, we implemented a multi-faceted approach:
- Gluten-Free Diet: Joseph eliminated gluten from his diet to reduce the inflammatory response triggered by his immune response to gluten and elevated anti-gliadin IgA.
- Increased Fermented Foods: Clinical trials have demonstrated the efficacy of fermented foods in boosting microbial diversity and reducing inflammation.3 Over a 10-week period, Joseph gradually introduced six daily servings of fermented foods, including yogurt, kefir, kimchi, and kombucha.
- Gradual Fiber Increase: While fiber alone doesn’t directly alter the microbiome, it helps support the growth and establishment of beneficial microbes. Fiber also aids in reducing fermentation-driven gas production by regulating motility.
- Probiotics and Prebiotics: These were introduced to further support gut health and aid in restoring balance.
Results and Progress
After three months, Joseph reported a 75% reduction in gas and belching. He no longer experienced nocturnal disruptions requiring bowel movements, and daytime bloating was virtually eliminated. The treatment also sparked a newfound interest in food diversity, with Joseph enthusiastically taking up home fermentation.
Looking ahead, the plan is to continue diversifying Joseph’s diet over the next three months to achieve further improvements in his symptoms.

Ilana Gurevich, ND, NSOM, FABNG
Dr. Gurevich is a naturopathic medical physician and an acupuncturist who uses individualized natural therapies to address the underlying cause of disease. She encourages her patients to take an active role in their own health care. Dr. Gurevich relies on a variety of natural modalities including Chinese and Western herbal medicine, acupuncture, nutritional supplements, homeopathy, hydrotherapy, and dietary education.
The opinions expressed in this presentation are the author's own. Information is provided for informational purposes only and is not meant to be a substitute for personal advice provided by a doctor or other qualified health care professional. Patients should not use the information contained herein for diagnosing a health or fitness problem or disease. Patients should always consult with a doctor or other health care professional for medical advice or information about diagnosis and treatment.
References
- Bull MJ, Plummer NT. Part 1: The Human Gut Microbiome in Health and Disease. Integr Med (Encinitas). 2014 Dec;13(6):17-22. PMID: 26770121; PMCID: PMC4566439.
- Napolitano M, Fasulo E, Ungaro F, Massimino L, Sinagra E, Danese S, Mandarino FV. Gut Dysbiosis in Irritable Bowel Syndrome: A Narrative Review on Correlation with Disease Subtypes and Novel Therapeutic Implications. Microorganisms. 2023 Sep 22;11(10):2369. doi: 10.3390/microorganisms11102369. PMID: 37894027; PMCID: PMC10609453.
- Wastyk HC, Fragiadakis GK, Perelman D, Dahan D, Merrill BD, Yu FB, Topf M, Gonzalez CG, Van Treuren W, Han S, Robinson JL, Elias JE, Sonnenburg ED, Gardner CD, Sonnenburg JL. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021 Aug 5;184(16):4137-4153.e14. doi: 10.1016/j.cell.2021.06.019. Epub 2021 Jul 12. PMID: 34256014; PMCID: PMC9020749.