Using the GI-MAP Stool Test to Uncover Parasitic Infections

A Healthy Lifestyle Meets Unexpected Challenges
Grace is a 42-year-old female that had always been very healthy and active. An avid cyclist, she would spend most of her leisure time biking and hiking in the backcountry. She was a long-standing patient who I would see one to two times a year for routine wellness and lab work.
The Onset of Unexplained Symptoms: A Sudden Change
When she walked into my office in June, she looked quite different than normal. She had lost a significant amount of weight, complained of fatigue, and reported a recent onset of abdominal pain. In March, she suddenly started experiencing upper and lower abdominal pain that initially was low grade and just in the upper abdomen.
Progression of Symptoms: From Bad to Worse
Over the next three months, Grace's pain increased in both intensity and location, eventually spreading to the lower abdomen. She reported pain that was always present but worsened three to five minutes after eating. Within 15 minutes of eating, the pain radiated to her right shoulder blade. Due to the increasing intensity of the pain, Grace was afraid to eat. In fact, the only time she was free of pain was when she was fasting. As a result, she lost an alarming 15 pounds three months before our visit. During these three-months, she also noticed a significant change in her bowel movements. Prior to March, Grace had always had one to two bowel movements daily that were complete and easy to pass. After March, she experienced significant constipation and began using laxatives to pass the stool. When she didn't use laxatives, she had three to four small, incomplete bowel movements per day that resembled rabbit-like pellets.
Seeking Medical Insight: Initial Diagnosis Efforts
As the pain continued to worsen, so did Grace's concern. After her initial visit, I referred Grace for an abdominal ultrasound to rule out cholecystitis, as many of the symptoms appeared similar. At that time, we also referred her to a gastroenterologist for a more comprehensive workup. The abdominal ultrasound found no abnormality of the gallbladder but did find a suspicious peripancreatic abnormality. We followed this up with a CT of the abdomen, which found nothing concerning in the pancreas but did find some inflammation of the jejunum. The gastroenterologist performed an endoscopy on Grace as well as a bile emptying HIDA scan. The endoscopy did not offer any new findings, and the gallbladder ejection fraction was only slightly lower than normal. The recommendation from the gastroenterologist was to proceed with a cholecystectomy and remove the gallbladder.
Questioning Surgical Intervention: Enter Functional Medicine and GI-MAP™
Grace questioned surgical intervention since no stones were found, and the ejection fraction was only slightly out of range. The gastroenterologist was not able to offer a reasonable answer as to why that was occurring and decided not to proceed with the surgery and see if functional medicine could help find the root cause of her symptoms. I ordered a GI-MAP for Grace to see if we could get more clarity on her intestinal heath and microbiome makeup.
Finding the Root Cause: GI-MAP Reveals Parasitic Infections
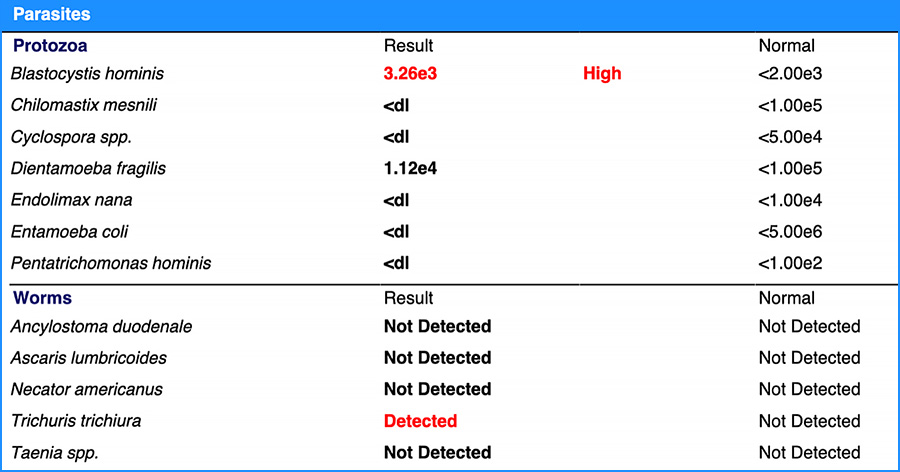
Thanks to the GI-MAP's quantitative PCR stool testing, we identified both the Trichuris trichiura worm and Blastocystis hominis on the parasites (protozoa) panel of the GI-MAP test. Trichuris trichiura is also known as human whipworm. The whipworm is an intestinal parasite that infects humans and is named for its worm's whip-like shape. The CDC explains the spread of whipworm as follows:
"Whipworms live in the intestine and whipworm eggs are passed in the feces of infected persons. If the infected person defecates outside—for example, near bushes, in a garden, or field—or if the feces of an infected person is used as fertilizer, then eggs are deposited on the soil. They can then grow into a form of the worm that can infect others."
CDC About Whipworm Infection 1
Infections of Trichuris trichiura can range from asymptomatic to severe, including abdominal pain and inflammation, blood and mucus in the stool, and diarrhea. Symptoms seem to depend both on the constitution of the infected person as well as the amount of worm burden they are carrying. Diagnosis is made from a stool sample, and quantitative PCR testing offers a more sensitive and specific way to detect the pathogen.2 The second parasite found on Grace's GI-MAP, Blastocystis hominis, can also provoke significant intestinal symptoms such as abdominal pain and discomfort, and constipation.
Connecting the Dots: Recalling the Backcountry Trip
After learning she had whipworm, Grace remembered that her symptoms started two weeks after going backcountry biking without a water filter. She had been wrongly informed that the water on the path was potable and drank it during her trip. The GI-MAP's identification of parasites helped Grace make the association between her trip and her illness.
A Targeted Treatment Approach: Combatting Parasitic Infections
Based on the GI-MAP results and the severity of her symptoms, I decided to treat Grace with antiparasitic medications. I used a combination therapy of Albendazole (400 mg) and Ivermectin (20 mcg/kg) daily for three days, and we repeated treatment two weeks later to guarantee we caught both life cycles of the worm.3
Trichuris trichiura takes 15 days to go from embryonate to an infective worm. I designed a protocol to catch both the embryo (egg) and the hatched worm and used antiparasitic medications to address both.
Successful Eradication of Parasites: Grace's Remarkable Recovery
Grace responded exceptionally well to this treatment. After a month, she reported a 90% improvement in her pain. Her bowel movements normalized, and her constipation greatly improved. She was able to return to her past diet and was able to gain back much of the weight she had lost during her illness. She became the biggest proponent of water filtration systems I have ever met. Her personal experience with whipworm solidified her commitment to clean filtered water.
Grace's story, punctuated by her ability to avoid unnecessary surgery, is another excellent example of why functional stool testing with GI-MAP can help find solutions for patients' symptoms and optimize clinical outcomes in my practice (and yours).

Ilana Gurevich, ND, NSOM, FABNG
Dr. Gurevich is a naturopathic medical physician and an acupuncturist who uses individualized natural therapies to address the underlying cause of disease. She encourages her patients to take an active role in their own health care. Dr. Gurevich relies on a variety of natural modalities including Chinese and Western herbal medicine, acupuncture, nutritional supplements, homeopathy, hydrotherapy, and dietary education.
REFERENCES
- CDC – About Whipworm Infection: www.cdc.gov/parasites/whipworm/gen_info/faqs.html
- Pilotte N, Papaiakovou M, Grant JR, Bierwert LA, Llewellyn S, McCarthy JS, Williams SA. Improved PCR-Based Detection of Soil Transmitted Helminth Infections Using a Next-Generation Sequencing Approach to Assay Design. PLoS Negl Trop Dis. 2016 Mar 30;10(3):e0004578.
- Clarke NE, Doi SAR, Wangdi K, Chen Y, Clements ACA, Nery SV. Efficacy of Anthelminthic Drugs and Drug Combinations Against Soil-transmitted Helminths: A Systematic Review and Network Meta-analysis. Clin Infect Dis. 2019 Jan 1;68(1):96-105. doi: 10.1093/cid/ciy423. PMID: 29788074.