Transforming Gastrointestinal Health with GI-MAP: A Case Study of Protozoa and SIgA

Sam's Journey: Unraveling Complex Health Issues
Sam is a 48-year-old male who presented to my clinic in a very ill state. He felt significantly older than his years and had multiple health issues that plagued him daily. Sam explained that over the last decade, he had numerous comprehensive workups by his primary care provider and various specialists. Frustratingly, they all came up empty-handed, and Sam continued to suffer.
Initial Assessment: Identifying the Core Symptoms
Gas, Bloating, and Food Intolerances
Sam's symptoms fell into three primary buckets – gastrointestinal (GI), fatigue, and urinary. After eating most meals, Sam suffered from gas and bloating and reported a worsening of his ability to function and perform day-to-day tasks.
Sam also reported numerous food intolerances and was following a very limited diet, ingesting just ten foods, which he tried to vary as much as possible. Any deviation from his highly restricted diet led to immediate abdominal pain and increased brain fog.
Unrelenting Fatigue
Sam's second major complaint was muscle tightness and fatigue. In his youth, Sam was a very active collegiate athlete. Now, just twenty years later, severe muscle fatigue impacted his ability to exercise. After an intense workout, he felt depleted and reported that it took him at least a week to recover. While Sam tried to push through the fatigue, he realized it was becoming non-sustainable.
Urinary Frequency
Sam woke up three to five times every night to urinate. The inability to sleep and rest well significantly impacted Sam's quality of life. As a result, his mood was often low or flat, and he suffered from significant brain fog.
GI-MAP Stool Test: A Step Towards Precision Diagnosis
On his first visit, Sam brought in a positive small intestinal bacterial overgrowth (SIBO) test that a different clinician had run. Despite being treated for SIBO multiple times with pharmaceuticals and herbs, he never experienced improvement. Skeptical of the diagnosis of SIBO, I chose to order a GI-MAP stool test for Sam. In my experience, GI-MAP can often reveal underlying causes of symptoms that mimic SIBO. Before GI-MAP, Sam had never had a large bowel assay outside of a non-remarkable culture and sensitivity test run through his general practitioner.
GI-MAP Reveals Underlying Causes: Protozoa, Low SIgA, and Elevated Zonulin
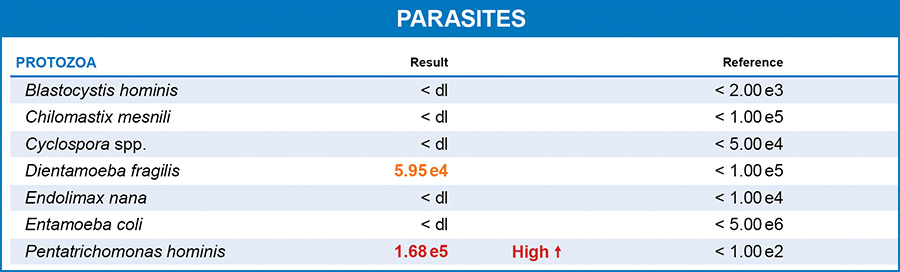
Sam's GI MAP results were surprising. He had a significant overgrowth of Pentatrichomonas hominis. Pentatrichomonas hominis is a flagellated protozoan that inhabits the large intestine of humans. This species was originally considered a commensal protozoan of the digestive tract but has recently been identified as a potential parasite and a causative agent of diarrhea.1 Infections of this parasite can lead to a condition called pentatrichomoniasis, which can cause symptoms such as diarrhea, abdominal pain, and other gastrointestinal discomforts. Pentatrichomonas hominis has also been associated with irritable bowel syndrome (IBS), systemic lupus erythematosus, and rheumatoid arthritis in humans.2 It has a correlation with colorectal cancers, and Pentatrichomonas hominis is present in the microbiome of many colorectal patients.3
Dientamoeba fragilis was also present in Sam's stool; however, it was below the lab reference range for high. In addition to the protozoa, Sam also had very low secretory immunoglobulin A (SIgA), indicating his immune system was functioning at below optimal levels. Plus, the GI-MAP showed Sam's zonulin levels were very highly elevated (nearly five times higher than the laboratory's upper limit.)
Addressing Protozoan Overgrowth: The Treatment Approach
My primary goal in treating Sam was to eradicate the protozoa. Currently, the Centers for Disease Control (CDC) has no treatment recommendations for Pentatrichomonas hominis. However, imidazole derivatives have shown some efficacy in the literature.4 In Sam's case, I prescribed Tinidazole for three days and repeated treatment two weeks later. Sam's GI-MAP showed a high-normal presence of Dientamoeba fragilis and Pentatrichomonas hominis. The literature shows that both are responsive to Tinidazole.5 Sam tolerated the treatment moderately well. During treatment, he experienced nausea, a worsening of his gas and diarrhea, as well as a strange metallic taste in his mouth. These symptoms resolved when he finished treatment.
Measurable Improvements and Ongoing Care
Sam and I checked in about three weeks and he reported a significant improvement. Sam's GI symptoms had vastly responded to treatment, and he experienced less gas, bloating, and pain. His sleep had marginally improved because his GI symptoms were less severe. He only woke up twice a night to urinate and could push a little harder and go a little longer during workouts.
The Importance of a Structured Treatment Strategy in GI Health
In my clinical practice, I always emphasize the importance of using a pyramid structure when treating multiple areas of gut dysfunction.
When a patient has positive GI-MAP findings for parasites and worms, I always prioritize the eradicating those species. A parasite, protozoa, or worm can change the GI environment in various ways.
Protozoa that inhabit the gastrointestinal tract directly interact with the GI microbiome. They compete for nutrients, alter the gut environment, and even feed on certain gut bacteria. This can lead to changes in the composition and diversity of the gut microbiome.6
Protozoa can also weaken the host's immune system (as indicated by Sam's low SIgA levels), allowing the host to be more susceptible to secondary bacterial and fungal infections, which can further alter the composition of the microbiome.7
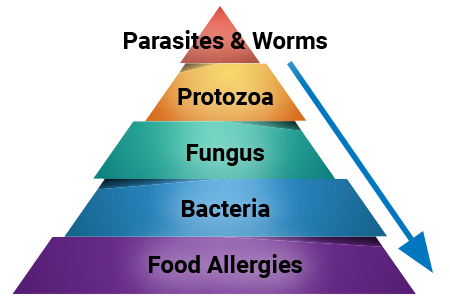
Finally, parasites may consume nutrients that would otherwise be available to the host or beneficial gut bacteria. This competition for nutrients can alter the balance of the microbiome, favoring certain microorganisms over others. This can make an environment that is more hospitable to the protozoa then it is to the host.8
Often, removing the protozoa from the GI is enough to improve the function of digestion and restore the patient to balance. Other times, we must do further work on the gut to restore health and resolve symptoms.
In Sam's case, getting rid of his protozoal infections was key to improving his overall health, but we also had to take significant steps to support his mucosal immune function and gut barrier integrity.
I treat complicated GI patients by going through the following steps.
- Discovering underlying causes and then eliminating pathogens
- Supporting the GI immune system
- Addressing intestinal permeability
Restoring Balance and Enhancing Quality of Life
Sam came into the clinic suffering, but we improved the function of his GI tract by using the abnormal findings presented in the GI-MAP and treating them accordingly. He can now participate fully in his life because his intestinal health has been restored.

Ilana Gurevich, ND, NSOM, FABNG
Dr. Gurevich is a naturopathic medical physician and an acupuncturist who uses individualized natural therapies to address the underlying cause of disease. She encourages her patients to take an active role in their own health care. Dr. Gurevich relies on a variety of natural modalities including Chinese and Western herbal medicine, acupuncture, nutritional supplements, homeopathy, hydrotherapy, and dietary education.
REFERENCES
- Maritz JM, Land KM, Carlton JM, Hirt RP. What is the importance of zoonotic trichomonads for human health? Trends Parasitol. 2014;30:333–341. – doi: 10.1016/j.pt.2014.05.005.
- Compaore C, Kemta Lekpa F, Nebie L, Niamba P, Niakara A. Pentatrichomonas hominis infection in rheumatoid arthritis treated with adalimumab. Rheumatology. 2013;52:1534–1535. – doi: 10.1093/rheumatology/kes38
- Zhang N, Zhang H, Yu Y, ect. High prevalence of Pentatrichomonas hominis infection in gastrointestinal cancer patients. Parasit Vectors. 2019 Aug 28;12(1):423. doi: 10.1186/s13071-019-3684-4
- Chomicz L, Padzik M, Laudy AE, et al. Anti-Pentatrichomonas hominis activity of newly synthetized benzimidazole derivates-in vitro studies, Acta Parasitol, 2009, vol. 54 (pg. 165-71)
- Nagata N, Marriott D, Harkness J, Ellis JT, Stark D. Current treatment options for Dientamoeba fragilis infections. Int J Parasitol Drugs Drug Resist. 2012 Sep 3;2:204-15. doi: 10.1016/j.ijpddr.2012.08.002.
- Berrilli F, Di Cave D, Cavallero S, D'Amelio S. Interactions between parasites and microbial communities in the human gut. Front Cell Infect Microbiol. 2012 Nov 16;2:141. doi: 10.3389/fcimb.2012.00141. PMID: 23162802;.
- Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014 Mar 27;157(1):121-41. doi: 10.1016/j.cell.2014.03.011. PMID: 24679531
- Pickard JM, Zeng MY, Caruso R, Núñez G. Gut microbiota: Role in pathogen colonization, immune responses, and inflammatory disease. Immunol Rev. 2017 Sep;279(1):70-89. doi: 10.1111/imr.12567. PMID: 28856738