Understanding SIgA on the GI-MAP: The Key Defender in the Immune Arsenal

About Secretory Immunoglobulin A (SIgA)
Secretory immunoglobulin A is the most abundant antibody in the body and is found in many mucus membranes. It comprises roughly 70 percent of the body's total immunoglobulins. The majority of IgA is found in the various mucous secretions, including saliva, milk, colostrum, tears, and secretions from the respiratory tract, genitourinary tract, and prostate.1 SIgA is the first line of defense against harmful microorganisms, such as bacteria, viruses, and parasites. Patients can become exposed to those pathogens by ingesting contaminated food or water or cooking on unclean, polluted surfaces. The role of SIgA is to bind to harmful pathogens and prevent them from attaching to and invading the gut's mucosal lining.
Elevated SIgA Levels: What Do They Signal?
There are many reasons why a patient might present with an elevated level of SIgA. The clinical picture of the patient, as well as findings from a GI-MAP™ test, are critical to finding the underlying cause(s). SIgA elevation can be transient or prolonged and, if prolonged, can indicate an ongoing immune response or underlying health condition. Elevated SIgA levels in the gastrointestinal (GI) tract can be a sign of the immune system's active defense against various challenges. While this immune response is generally protective, persistently elevated levels could be indicative of underlying conditions or chronic inflammation.2 The presence of pathogens, including bacteria, viruses, parasites, and fungi, can stimulate the production of SIgA in the GI lumen. The SIgA traps and neutralizes these invaders.3 We also see an elevated SIgA as a marker for other chronic diseases, such as celiac disease and inflammatory bowel disease (IBD). The inflammatory process can trigger an increase in SIgA production as the immune system attempts to combat the ongoing inflammation. Other factors that can increase SIgA include exposure to food allergies, environmental toxins, food additives, or foods that irritate the gastrointestinal (GI) tract.4
Low SIgA: A Marker of Compromised Immune Health
A suppressed SIgA is often associated with a compromised mucosal immune system. Prolonged chronic GI organic diseases like celiac disease and inflammatory bowel disease can lead to a suppressed SIgA if the inflammatory process continues unhindered. SIgA becomes suppressed with chronic infections within the gut. The immune system may become overburdened in its effort to combat the persistent infection.5,6 This can contribute to problems like increased gut permeability and susceptibility to other gastrointestinal infections, which can lead to even further dysbiosis.
Sam's Journey: Protozoa Infections and Suppressed SIgA Level
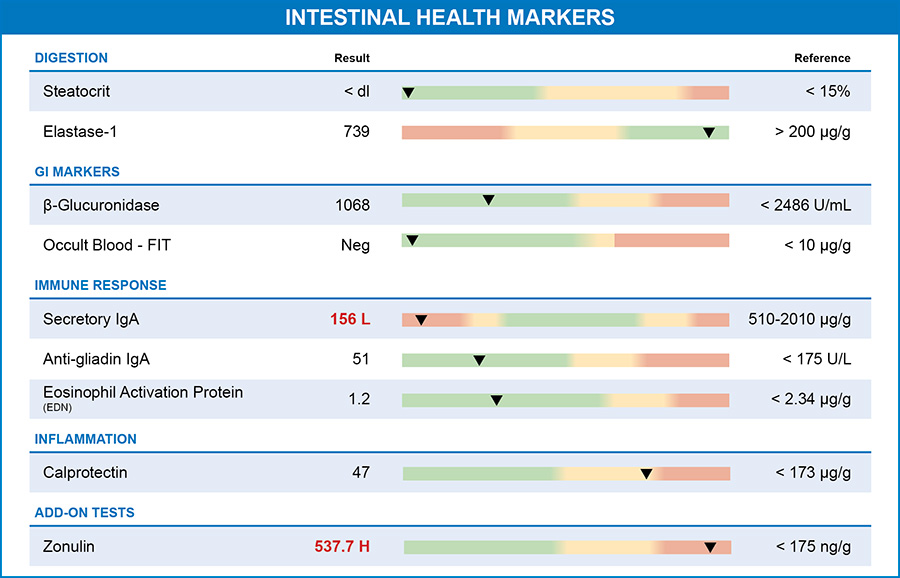
Sam came to the clinic to see me after having felt unwell for quite some time. I ordered a GI-MAP test with the Zonulin Add-On to get a complete picture of his gut health. When looking at Sam's GI-MAP test, the immune system dysregulation was evident. His SIgA level was extremely low. His GI-MAP also identified two protozoa in Sam's stool. Sam's low SIgA levels are not surprising, given that his health issues were long-standing, and the protozoa were most likely present for a long time.
When addressing either an elevation or a suppression of SIgA, I prioritize identifying the underlying cause. I use the GI-MAP because it quantitatively detects protozoa or parasitic infections, bacterial overgrowth of dysbiotic species, and fungal overgrowth. In my practice, I address the protozoa (or other infections) before targeting the SIgA. After they are eradicated, I help patients rebuild their GI immune system.
Strategies for Optimizing SIgA Levels: From Diet to Probiotics
Focusing on living a clean lifestyle can help boost SIgA levels. I encourage my patients to eat a diet high in whole, non-processed foods and avoid foods contaminated with herbicides and pesticides. Supporting the GI with prebiotic fibers and probiotics in fermented food is also an effective strategy. Stress management is also key. Chronic stress can negatively impact the gut and the immune system, potentially suppressing the SIgA levels. Stress-reduction techniques like mindfulness, yoga, meditation, or deep breathing exercises have been shown to regulate the SIgA of the gastrointestinal tract.7
Data also supports the use of high-dose probiotics. Multiple randomized control trials found an increase in SIgA after utilizing multi-strain probiotics for various conditions, including GI disorders and also conditions like severe burns.8 One randomized control trial showed efficacy for children hospitalized for acute gastroenteritis. They found benefit from a lactobacillus-based probiotic.9 Finally, many papers have found that probiotics support the normal function of SIgA. Probiotics stabilize the GI immune system in several ways, including inhibiting the growth of pathogenic bacteria. Probiotics outcompete pathogens in the use of nutrients for growth and proliferation. Several studies have shown Lactobacillus rhamnosus strain GG, and L. plantarum exhibited the ability to inhibit attachment of enteropathogenic Escherichia coli in the GI tract.10
Glutamine and Quercetin: Nourishing the Immune System
Glutamine is also a very reliable nutrient to support SIgA. Glutamine is the most abundant and versatile amino acid in the body. The rate of glutamine consumption by immune cells is similar to or greater than glucose. While the body typically synthesizes it, there are situations in which the body's demand for glutamine exceeds its production capacity. Glutamine is a primary energy source for rapidly dividing cells, including immune cells. It provides the necessary energy for immune cells to carry out their functions effectively. This energy is crucial for mounting immune responses to infections and maintaining immune cell activity in the gut.11
Finally, quercetin is a valuable tool in supporting the optimal function of the GI tract. Quercetin is a natural bioflavonoid compound found in many fruits, vegetables, and plants. Quercetin has been found to modulate the activity of immune cells. This modulation can promote a balanced and appropriate immune reaction in the gut.12 Another human study that specifically looked at LPS (lipopolysaccharide) showed that quercetin suppresses the inflammatory response caused by LPS endotoxin, which then supports immune function in the GI tract.13
Integrating Natural Medicine: Sam's Path to GI Wellness
Once Sam's gut had healed from the protozoa, I used the naturopathic tools above to address his low levels of SIgA. I rely on the GI-MAP test in practice because it helps me pinpoint the root causes of GI and immune dysfunction. I then personalize protocols incorporating lifestyle changes, dietary adjustments, and nutraceutical tools to restore the body to healthy physiology.

Ilana Gurevich, ND, NSOM, FABNG
Dr. Gurevich is a naturopathic medical physician and an acupuncturist who uses individualized natural therapies to address the underlying cause of disease. She encourages her patients to take an active role in their own health care. Dr. Gurevich relies on a variety of natural modalities including Chinese and Western herbal medicine, acupuncture, nutritional supplements, homeopathy, hydrotherapy, and dietary education.
REFERENCES
- The biology of intestinal immunoglobulin A responses. Cerutti A, Rescigno Immunity. 2008;28(6):740.
- Mantis NJ, Rol N, Corthésy B. Secretory IgA's complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunol. 2011 Nov;4(6):603-11. doi: 10.1038/mi.2011.41. Epub 2011 Oct 5. PMID: 21975936;
- Pietrzak B, Tomela K, Olejnik-Schmidt A, Mackiewicz A, Schmidt M. Secretory IgA in Intestinal Mucosal Secretions as an Adaptive Barrier against Microbial Cells. Int J Mol Sci. 2020 Dec 4;21(23):9254. doi: 10.3390/ijms21239254. PMID: 33291586
- Mantis NJ, Forbes SJ. Secretory IgA: arresting microbial pathogens at epithelial borders. Immunol Invest. 2010;39(4-5):383-406. doi: 10.3109/08820131003622635. PMID: 20450284.
- Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017 Sep;11(9):821-834. doi: 10.1080/17474124.2017.1343143. Epub 2017 Jun 26. PMID: 28650209.
- Amimo JO, Michael H, Chepngeno J, Raev SA, Saif LJ, Vlasova AN. Immune Impairment Associated with Vitamin A Deficiency: Insights from Clinical Studies and Animal Model Research. Nutrients. 2022 Nov 26;14(23):5038. doi: 10.3390/nu14235038. PMID: 36501067.
- Househam AM, Peterson CT, Mills PJ, Chopra D. The Effects of Stress and Meditation on the Immune System, Human Microbiota, and Epigenetics. Adv Mind Body Med. 2017 Fall;31(4):10-25. PMID: 29306937.
- Saputro ID, Putra ON, Pebrianton H, Suharjono. Effects of probiotic administration on IGA and IL-6 level in severe burn patients: a randomized trial. Ann Burns Fire Disasters. 2019 Mar 31;32(1):70-76. PMID: 31285738
- Freedman SB, Horne R, Johnson-Henry K, et. Al. Pediatric Emergency Research Canada Probiotic Regimen for Outpatient Gastroenteritis Utility of Treatment (PROGUT) Trial Group. Probiotic stool secretory immunoglobulin A modulation in children with gastroenteritis: a randomized clinical trial. Am J Clin Nutr. 2021 Apr 6;113(4):905-914. doi: 10.1093/ajcn/nqaa369.
- Maldonado Galdeano C, Cazorla SI, Lemme Dumit JM, Vélez E, Perdigón G. Beneficial Effects of Probiotic Consumption on the Immune System. Ann Nutr Metab. 2019;74(2):115-124. doi: 10.1159/000496426. Epub 2019 Jan 23
- Cruzat V, Macedo Rogero M, Noel Keane K, Curi R, Newsholme P. Glutamine: Metabolism and Immune Function, Supplementation and Clinical Translation. Nutrients. 2018 Oct 23;10(11):1564. doi: 10.3390/nu10111564. PMID: 30360490
- Medoro A, Davinelli S, Colletti A, Di Micoli V, Grandi E, Fogacci F, Scapagnini G, Cicero AFG. Nutraceuticals as Modulators of Immune Function: A Review of Potential Therapeutic Effects. Prev Nutr Food Sci. 2023 Jun 30;28(2):89-107. doi: 10.3746/pnf.2023.28.2.89. PMID: 37416796
- Zhang M, Lin JM, Li XS, Li J. Quercetin ameliorates LPS-induced inflammation in human peripheral blood mononuclear cells by inhibition of the TLR2-NF-κB pathway. Genet Mol Res. 2016 Jul 14;15(2). doi: 10.4238/gmr.15028297. PMID: 27421015.