GI-MAP and IgG Food Explorer: The Best Tests for Identifying Food Sensitivities in Functional Medicine

In functional medicine, identifying the root causes of food sensitivities is essential for improving digestion, mood, immune resilience, and overall health. While elimination diets have their place, they often fail to fully address why a patient reacts to food.
That’s where the GI-MAP® and IgG Food Explorer™ become a powerful diagnostic duo to help practitioners move beyond guesswork and toward data-driven, personalized protocols.
What Is the IgG Food Explorer Test?
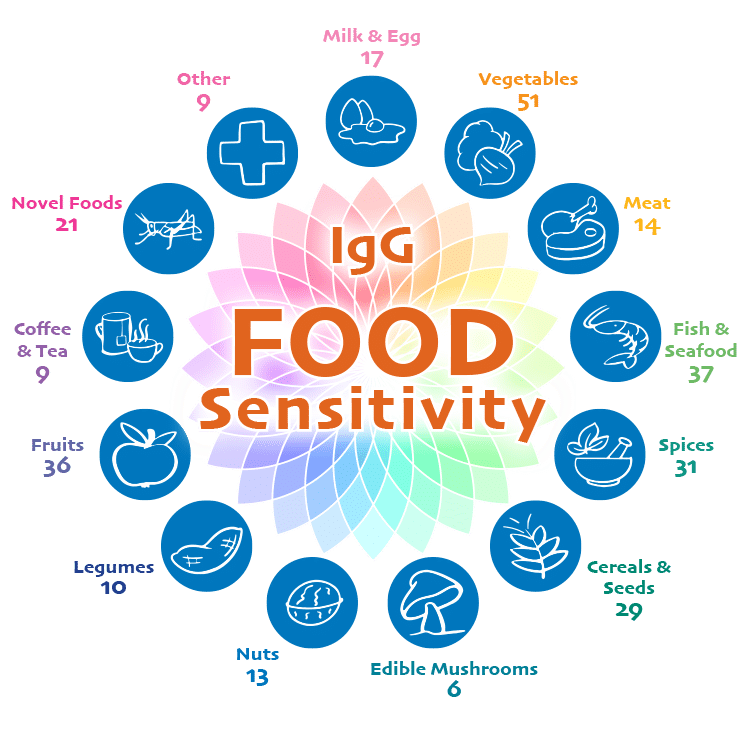
 The IgG Food Explorer is a comprehensive IgG food sensitivity test measuring antibodies to 250+ food antigens. It can be collected through a simple at-home collection kit or standard phlebotomy.
The IgG Food Explorer is a comprehensive IgG food sensitivity test measuring antibodies to 250+ food antigens. It can be collected through a simple at-home collection kit or standard phlebotomy.
This test is especially valuable because:
- Up to 20% of people in industrialized nations report adverse food reactions¹
- Up to 60% of patients with functional GI disorders experience food-related symptoms¹
The panel includes:
- 5 gluten-specific antigens, including the Tri a Gliadin molecular antigen
- A full dairy antigens profile, including molecular antigens to differentiate between responses to casein and whey
- Common and uncommon food triggers
- Additives and hidden dietary components
This level of specificity helps practitioners make accurate dietary recommendations instead of removing foods indefinitely.
Symptoms That Suggest Food Sensitivities
Food sensitivities can manifest in surprising ways. Patients often present with symptoms that seem unrelated until testing reveals the underlying pattern.
Common symptoms of food sensitivities include:
- Bloating, gas, constipation, diarrhea
- Skin rashes, eczema, hives
- Weight gain or weight loss resistance
- Joint pain or inflammation
- Migraines and headaches
- Anxiety, depression, mood swings
- Fatigue and brain fog
- Neurological changes such as ataxias
When symptoms remain unexplained or persist beyond standard treatment, IgG testing becomes essential.
GI-MAP: The Gut–Immune Link Behind Food Sensitivities
 The GI-MAP offers critical insights that explain why the immune system has a heightened reaction to foods. It evaluates:
The GI-MAP offers critical insights that explain why the immune system has a heightened reaction to foods. It evaluates:
- Gut microbiome balance
- Opportunistic or pathogenic organisms
- Commensal diversity
- Digestive insufficiencies
- Intestinal permeability
- Inflammation markers
This allows practitioners to correlate gut dysfunction with IgG reactions, giving a complete picture of root-cause dysfunction. For example, infections and alterations in commensal bacterial balance have been linked with immune dysregulation and heightened responses to dietary antigens.²
Why GI-MAP + IgG Food Explorer Work Better Than Elimination Diets
Elimination diets often:
- Miss hidden or delayed reactions
- Don’t fully address underlying gut problems
- Lead to overly restrictive eating
- Fail to restore oral (immune) tolerance
When combined, GI-MAP and IgG testing provide:
- A clear map of dietary triggers
- Insight into gut permeability and reduced digestive capacity
- Identification of dysbiosis contributing to food reactions
- The ability to prioritize which foods to remove and which to reintroduce
- A path to improving immune tolerance over time
This is the true functional medicine approach to addressing food sensitivities.
How to Use GI-MAP and IgG Testing to Improve Patient Outcomes
When used together, the GI-MAP and IgG Food Explorer give practitioners a complete clinical picture—moving patient care beyond symptom-driven elimination diets and toward true immune recalibration. Here’s what this integrated approach allows you to do:
- Address Gut Barrier Dysfunction (Leaky Gut)
The GI-MAP identifies intestinal permeability markers such as zonulin and highlights dysbiosis patterns known to compromise the epithelial barrier. Zonulin is a key regulator of intestinal tight junctions, and elevations reflect increased gut permeability.³
This makes it possible to prioritize:
- Temporarily reducing exposure to high-reactive foods
- Gut healing protocols
- Supporting mucosal immunity (Secretory IgA)
- Microbiome balance and short chain fatty acid (SCFA) production
- Improve Digestion and Nutrient Assimilation
GI-MAP signals like low elastase, steatocrit, and disrupted microbiome diversity and overgrowth can explain why patients react to foods in the first place.
When digestion is incomplete, large food antigens reach the immune system intact, driving IgG reactions. Practitioners can support digestive capacity by addressing:
- Stomach acid
- Pancreatic and/or small intestine brush border enzymes
- Bile flow
- Motility
- Reduce Systemic and Mucosal Inflammation
IgG elevations often mirror underlying inflammation. GI-MAP markers such as calprotectin, secretory IgA, and microbiome overgrowths give practitioners the context needed to address systemic inflammatory drivers.
When inflammation is resolved, food reactions may naturally diminish.
- Restore Oral Tolerance
This is the true goal of food sensitivity treatment.
Food sensitivities are not just about the foods themselves. They reflect:
- Disrupted mucosal integrity
- Repeated exposure to the same antigens
- Impaired immune tolerance training
- Microbiome imbalance
By reducing immune burden and repairing the gut, practitioners help patients retrain the immune system to tolerate foods again.
- Create Safe, Structured Food Reintroductions
With clear antibody data, reintroduction becomes strategic, not guesswork. Practitioners can:
- Avoid unnecessary restrictions
- Stagger food trials
- Track symptoms alongside IgG trends
- Reintroduce nutrient-dense foods once the gut is healed
- This gives patients back the foods they miss, and the nutrition they need.
- End the Cycle of Unnecessary Food Restriction
Without testing, elimination diets can become endless and overly restrictive.
By combining GI-MAP and IgG results, practitioners can confidently:
- Identify true reactive foods
- Avoid the trap of “removing everything”
- Give patients a path toward dietary freedom, not lifelong avoidance
The Real Goal: Immune Calm, Not Lifelong Avoidance
The goal of food sensitivity care is not to shrink a patient’s diet—it is to reduce immune activation, restore gut integrity, and help patients regain tolerance over time.
By addressing the root causes of food reactions, rather than simply eliminating foods, practitioners can help patients reduce symptoms, strength overall gut resilience, and support long-term immune balance.
Additional Resources

Diagnostic Solutions Laboratory
Brought to you by the Diagnostic Solutions Laboratory team. Our commitment is to serve the clinical needs of the health care provider with cutting-edge laboratory medicine by utilizing proven methodologies that are accurate and reliable.
The opinions expressed in this presentation are the author's own. Information is provided for informational purposes only and is not meant to be a substitute for personal advice provided by a doctor or other qualified health care professional. Patients should not use the information contained herein for diagnosing a health or fitness problem or disease. Patients should always consult with a doctor or other health care professional for medical advice or information about diagnosis and treatment.
- Onyimba F, Crowe SE, Johnson S, Leung J. Food Allergies and Intolerances: A Clinical Approach to the Diagnosis and Management of Adverse Reactions to Food. Clin Gastroenterol Hepatol. 2021;19(11):2230-2240.e1. doi:10.1016/j.cgh.2021.01.025
- Caminero A, Meisel M, Jabri B, Verdu EF. Mechanisms by which gut microorganisms influence food sensitivities. Nat Rev Gastroenterol Hepatol. 2019;16(1):7-18. doi:10.1038/s41575-018-0064-z
- Fasano A. Zonulin, regulation of tight junctions, and autoimmune diseases. Ann NY Acad Sci. 2012.